Paresthesia can be an unnerving experience, leaving many to wonder what’s happening within their bodies. Whether it’s a fleeting tingling sensation in your fingers or persistent numbness that disrupts daily life, understanding the differences between transient and chronic paresthesia is vital.
These two forms of paresthesia may share similar symptoms but stem from very different causes and implications. By deciphering these nuances, you can better navigate your health journey and make informed decisions about treatment options. Let’s dive deeper into the world of paresthesia to uncover what sets transient apart from chronic experiences.
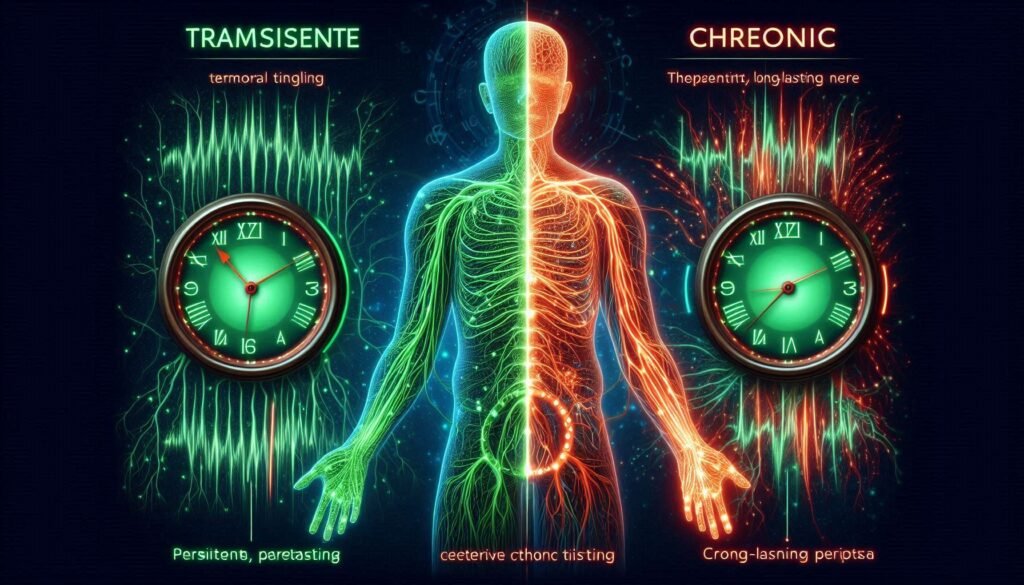
Defining Transient and Chronic Paresthesia
Paresthesia refers to abnormal sensations such as tingling, prickling, or numbness. It can occur anywhere in the body but is commonly felt in the limbs. Transient paresthesia is characterized by brief episodes that typically resolve quickly without any lasting effects. This type often arises from temporary nerve compression or other short-lived triggers.
Chronic paresthesia, on the other hand, persists for extended periods—often three months or longer. Its symptoms can vary in intensity and may be linked to underlying medical conditions affecting the nervous system. Chronic cases often signal something more serious that requires attention.
The causes of these two types differ significantly as well. While transient paresthesia might result from sitting awkwardly or a minor injury, chronic paresthesia could indicate issues such as diabetes, multiple sclerosis, or neuropathy.
Understanding these definitions helps individuals recognize their experiences with paresthesia better and seek appropriate care when necessary.
Causes of Transient Paresthesia: Common Triggers
Transient paresthesia often stems from temporary factors that disrupt nerve function. One common trigger is compression of nerves, which can occur when sitting or lying in one position for too long. This pressure can lead to sensations like tingling or numbness, typically resolving once the position changes.
Another frequent cause involves exposure to cold temperatures. Cold environments can constrict blood vessels and diminish circulation, resulting in a fleeting feeling of pins and needles. Once warmed up, these sensations usually dissipate quickly.
Certain activities also play a role; repetitive motions such as typing or playing an instrument may strain muscles around nerves, leading to transient symptoms. These are more prevalent during prolonged tasks without breaks.
Additionally, anxiety and stress might contribute by causing hyperventilation or muscle tension—which can affect nerve sensitivity. Recognizing these triggers helps individuals manage their symptoms effectively without panic.
Chronic Paresthesia: Underlying Conditions and Risk Factors
Chronic paresthesia often signals underlying health issues that require attention. Conditions such as diabetes, multiple sclerosis, and stroke frequently contribute to this persistent sensation. Each of these disorders affects nerve function in different ways, leading to ongoing tingling or numbness.
Autoimmune diseases can also play a significant role. Conditions like lupus or rheumatoid arthritis cause inflammation that may damage nerves over time. This damage results in chronic sensations that can be both distressing and debilitating for individuals affected.
In addition to medical conditions, certain lifestyle factors increase the risk of developing chronic paresthesia. Prolonged alcohol use can lead to peripheral neuropathy, while vitamin deficiencies—especially B12—can hinder nerve health.
Age is another critical factor; older adults are more likely to experience chronic paresthetic symptoms due to natural wear on the nervous system. Understanding these connections between underlying conditions and risk factors helps in recognizing when intervention might be necessary.
Duration and Frequency: Key Distinguishing Factors
Duration and frequency are crucial in differentiating between transient and chronic paresthesia. Transient paresthesia often occurs as a temporary sensation, lasting only seconds to minutes. It can happen after awkward positioning or pressure on nerves, such as when your leg “falls asleep.”
On the other hand, chronic paresthesia persists over longer periods—often for months or even years. This ongoing condition is usually linked to underlying health issues that require medical attention. The sensations may come and go but remain more frequent than those of transient episodes.
Individuals experiencing transient paresthesia typically find relief quickly by changing positions or shaking out limbs. In contrast, those with chronic symptoms might endure them daily without significant improvement through simple adjustments.
Understanding these duration and frequency patterns helps healthcare providers assess severity and potential causes effectively. Properly identifying whether a patient experiences fleeting sensations or continuous discomfort is essential for accurate diagnosis and treatment planning.
Symptom Patterns in Transient vs. Chronic Paresthesia
Paresthesia manifests differently based on whether it is transient or chronic. Transient paresthesia typically presents as brief episodes of tingling, numbness, or a prickly sensation. These sensations can occur after pressure on nerves, such as sitting with legs crossed for too long or sleeping in an awkward position. The symptoms usually resolve quickly once the pressure is relieved.
Chronic paresthesia, however, tends to be more persistent and may last for weeks or even longer. Individuals often describe these feelings as continuous tingling or burning sensations that do not easily subside. This form may also include changes in skin sensitivity—some areas may become hypersensitive while others feel less responsive.
Additionally, chronic cases can present alongside other neurological symptoms like weakness or difficulty coordinating movements. This broader array of symptoms distinguishes chronic paresthesia from its transient counterpart.
While both types involve unusual sensations, the duration and intensity are crucial factors that help differentiate between them. Recognizing these patterns aids in identifying the underlying cause and determining appropriate management strategies.
Diagnostic Approaches for Differentiating Transient and Chronic Forms
When it comes to diagnosing transient vs. chronic paresthesia, healthcare providers rely on a thorough assessment of symptoms and medical history. Understanding the duration and frequency of episodes is crucial here. Transient cases often occur in brief bursts, while chronic conditions may present with persistent or recurrent sensations.
Physical examinations play a significant role as well. Doctors will check for any signs of nerve damage or neurological disorders by testing reflexes, muscle strength, and sensory responses. These evaluations help narrow down potential causes.
Diagnostic imaging techniques such as MRI or CT scans can be employed if structural abnormalities are suspected. Blood tests may also be conducted to rule out metabolic issues like diabetes or vitamin deficiencies that could contribute to paresthetic sensations.
Electromyography (EMG) studies provide additional insights into nerve function and can differentiate between various underlying conditions causing paresthesia. This comprehensive approach aids in accurately categorizing the type of paresthesia experienced by the patient.
Treatment Strategies for Transient Paresthesia
Treatment strategies for transient paresthesia often focus on addressing the underlying causes. If the condition is triggered by pressure on nerves, simple adjustments can help alleviate symptoms. Shifting positions or taking breaks during prolonged activities may reduce discomfort and restore normal sensation.
In cases where anxiety or panic attacks induce paresthesia, calming techniques like deep breathing exercises can be effective. Mindfulness practices and cognitive-behavioral therapy also offer valuable tools to manage stress-related triggers.
If nutrient deficiencies contribute to the episodes, dietary changes or supplements might be necessary. Ensuring adequate intake of vitamins B12 and D can support nerve health and function.
For individuals experiencing recurrent transient paresthesia due to certain medical conditions, working closely with a healthcare professional is key. They can provide tailored advice and recommend lifestyle modifications that promote better overall nerve health while minimizing flare-ups.
Managing Chronic Paresthesia: Long-Term Approaches
Managing chronic paresthesia requires a multifaceted approach tailored to individual needs. Patients often work closely with healthcare providers to address underlying conditions contributing to their symptoms. This may involve treating diabetes, multiple sclerosis, or other neurological disorders that can lead to persistent sensations.
Physical therapy is another valuable strategy. A trained therapist can design exercises aimed at improving circulation and nerve function. Regular physical activity also helps maintain mobility and reduces discomfort associated with chronic paresthesia.
Medications might be prescribed for symptom relief as well. Options include pain relievers, anti-inflammatory drugs, or medications specifically targeting nerve pain such as gabapentin or pregabalin. These can help manage day-to-day challenges effectively.
Additionally, lifestyle changes play a crucial role in managing symptoms long-term. Stress reduction techniques like mindfulness meditation and yoga are beneficial for many patients, while dietary adjustments may improve overall health and contribute to reduced paresthetic episodes.
Impact on Quality of Life: Transient vs. Chronic Paresthesia
The impact of paresthesia on quality of life varies significantly between its transient and chronic forms. Transient paresthesia is often brief, triggered by specific activities or positions like sitting cross-legged for too long. While uncomfortable, it typically resolves quickly without major disruption to daily life.
In contrast, chronic paresthesia can be a persistent source of discomfort. Individuals may experience tingling or numbness regularly, which can interfere with routine tasks such as typing, driving, or even simple movements. This ongoing challenge may lead to frustration and decreased productivity.
Moreover, the emotional toll should not be underestimated. People dealing with chronic symptoms might find themselves anxious about their condition worsening or affecting their social interactions. This anxiety can exacerbate feelings of isolation and stress.
The distinction in quality of life impacts highlights the importance of understanding these two types of paresthesia. By recognizing how they differ in duration and effect on daily living, individuals can better advocate for their health needs.
When to Worry: Red Flags in Both Types of Paresthesia
While understanding transient vs. chronic paresthesia can help you identify and manage your symptoms, knowing when to seek medical attention is crucial. For transient paresthesia, if the sensation persists longer than a few minutes or occurs frequently, it’s wise to consult a healthcare provider.
On the other hand, chronic paresthesia may indicate underlying health issues that require urgent attention. Watch for signs such as sudden onset after an injury, weakness in limbs, or significant changes in vision or speech. These could signal more serious conditions like stroke or nerve damage.
Always take note of any accompanying symptoms like pain radiating from the affected area or unusual sensations spreading beyond one location on your body. Keeping track of how often these episodes occur and under what circumstances can provide valuable information for your doctor.
If you’re experiencing confusion about whether your symptoms are transient or chronic—and especially if they’re worsening—it’s essential to get evaluated by a professional who can guide you toward appropriate treatment options tailored to your specific condition and needs. Safeguarding your health starts with awareness and timely action regarding these important signals from your body.


