Paresthesia can be a perplexing condition, often presenting as unusual sensations like tingling, numbness, or a crawling feeling on the skin. Whether it’s your fingers, toes, or any other body part affected, understanding how these symptoms evolve is crucial for effective management. Many individuals may find themselves wondering: What does it mean when these sensations change? How do I know if my paresthesia is progressing?
In this guide, we’ll explore the progression of paresthesia symptoms—what to expect at each stage and practical tips on managing them. By recognizing early signs and understanding patterns of progression, you empower yourself to take control of your health journey. Let’s delve into the intricacies of this condition so that you can navigate its complexities with confidence and clarity.
Early Stages: Recognizing Initial Paresthesia Symptoms
The early stages of paresthesia often start with subtle, fleeting sensations. You might notice a tingling feeling in your fingers or toes, sometimes described as “pins and needles.” This sensation can occur after staying in one position for too long or during physical activities that compress nerves.
As the condition progresses, these initial symptoms may become more pronounced. You could experience numbness that lasts longer than just a few moments. While it can be alarming, recognizing these signs early is essential for effective management and intervention.
Some individuals report feelings of warmth or coldness in specific areas without any apparent cause. These atypical sensations are key indicators of nerve involvement and should not be ignored. Monitoring how frequently they occur can help you track changes over time.
It’s important to consider accompanying factors such as fatigue or stress levels since they may exacerbate symptoms. Being aware of these initial signs allows for timely discussions with healthcare providers about potential underlying causes and treatments.
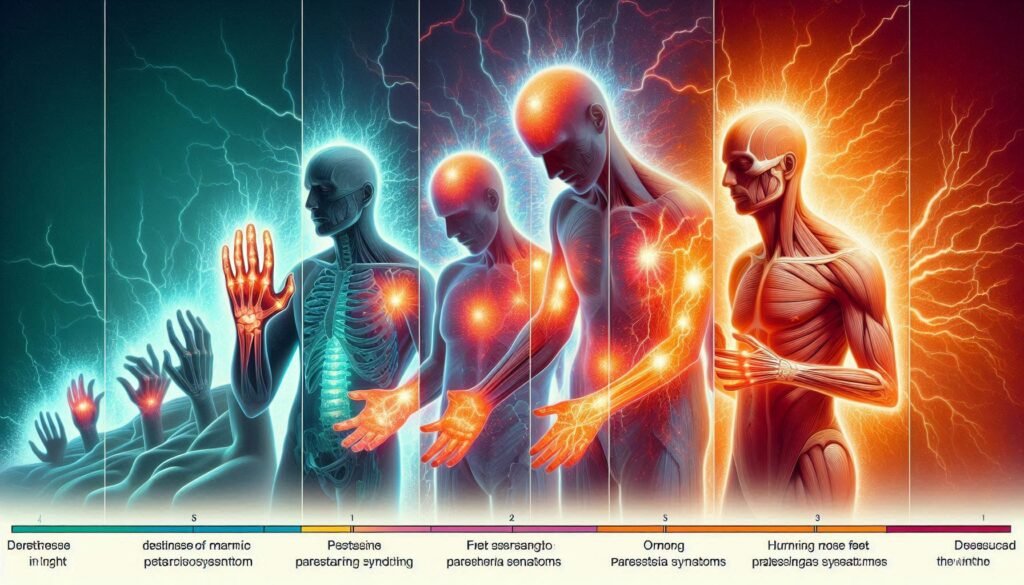
Patterns of Progression: Common Trajectories in Paresthesia
Paresthesia symptoms can vary greatly from one person to another, but certain patterns often emerge. Initially, many individuals experience tingling or numbness in localized areas, frequently affecting the hands and feet. This sensation may come and go sporadically.
As time progresses, these sensations might become more persistent. In some cases, people report a gradual increase in intensity or frequency of the symptoms. Discomfort can also shift from one area of the body to another as nerve irritation evolves.
Others might notice that paresthesia is triggered by specific activities or positions. For example, sitting for long periods could exacerbate symptoms in the legs while other movements relieve them temporarily.
Understanding these common trajectories helps patients anticipate changes in their condition. Recognizing when paresthesia begins to change allows for proactive management strategies tailored to individual experiences and needs.
Factors Influencing Symptom Progression
Various factors can influence the progression of paresthesia symptoms. One significant element is the underlying cause of the condition. For instance, diabetes and nerve damage may lead to more severe and rapid symptom development compared to other causes like temporary compression.
Lifestyle choices also play a crucial role. Poor nutrition, lack of exercise, and unhealthy habits such as smoking or excessive alcohol consumption can exacerbate symptoms. Addressing these lifestyle factors often helps manage symptom severity.
Additionally, comorbidities impact how quickly symptoms progress. Conditions like multiple sclerosis or vitamin deficiencies may interact with paresthesia, creating overlapping effects that intensify discomfort over time.
Emotional health should not be overlooked. Stress and anxiety can heighten sensitivity to pain or discomfort associated with paresthesia. Managing mental well-being through relaxation techniques or therapy might alleviate some symptom burdens as part of a comprehensive treatment plan.
Acute vs. Chronic Paresthesia: Understanding the Timeline
Paresthesia can manifest in two distinct forms: acute and chronic. Acute paresthesia is typically temporary, often arising from pressure on nerves or minor injuries. This form may present as tingling or “pins and needles” sensations that resolve quickly once the underlying cause is addressed, such as changing positions.
On the other hand, chronic paresthesia persists longer than a few months and can indicate underlying health issues. Conditions like diabetes, multiple sclerosis, or neuropathy are common culprits of this enduring experience. Symptoms might fluctuate but generally remain consistent over time.
The timeline between these two forms varies significantly. Acute symptoms tend to dissipate relatively fast with appropriate care. Conversely, chronic symptoms require ongoing management strategies to alleviate discomfort effectively.
Understanding the difference between acute and chronic paresthesia is crucial for proper diagnosis and treatment planning. Recognizing how long symptoms last helps guide further investigation into potential root causes and tailored therapies needed for relief.
Warning Signs of Accelerated Progression
Accelerated progression of paresthesia can be concerning. Being aware of warning signs is crucial for timely intervention. Sudden increases in numbness or tingling may indicate a shift in your condition that requires attention.
Another red flag is the emergence of new symptoms, such as muscle weakness or coordination issues. These changes could suggest underlying nerve damage and might necessitate further evaluation by a healthcare professional.
Additionally, if you notice persistent pain alongside your usual paresthesia, this could signal worsening nerve irritation or injury. Tracking these variations helps create a clearer picture for both you and your doctor.
If episodes become more frequent or last longer than before, it’s essential to seek medical guidance. Early detection can lead to better management strategies and potentially slow down the progression of symptoms.
Complications and Secondary Symptoms Over Time
Paresthesia symptoms can evolve over time, leading to various complications that affect daily life. Initially, tingling and numbness may seem benign. However, as these sensations persist or worsen, they can lead to more significant issues such as impaired mobility or reduced dexterity.
Chronic paresthesia might also trigger emotional responses like anxiety and depression. As individuals grapple with persistent discomfort or uncertainty about their condition’s progression, mental health can take a hit. This emotional strain often exacerbates the physical symptoms.
In some cases, long-term paresthesia can result in muscle weakness or atrophy due to disuse. When sensation is compromised, patients may avoid using affected limbs for fear of injury or further pain. Consequently, this avoidance leads to decreased strength and function.
Additionally, underlying conditions contributing to paresthesia—such as diabetes or neuropathy—may progress if not managed effectively. The interplay between primary symptoms and secondary complications underscores the importance of monitoring changes diligently.
Monitoring Tools: Tracking Paresthesia Progression
Monitoring the progression of paresthesia symptoms is essential for effective management. Various tools and methods can help individuals track changes and identify patterns over time. Journaling is one of the simplest yet most effective ways to document daily experiences, including symptom intensity, duration, and specific triggers.
There are also apps designed specifically for monitoring health conditions. These digital tools often allow users to input their symptoms easily and analyze trends through visual charts. Such features can provide valuable insights that may not be immediately apparent.
Wearable technology has gained traction as well. Devices like smartwatches or fitness trackers can monitor physiological metrics such as heart rate or activity levels, which may correlate with paresthesia episodes.
Regular communication with healthcare providers enhances this tracking process too. Sharing documented data helps practitioners tailor treatment plans based on real-time information about symptom progression.
Treatment Adjustments: Adapting to Changing Symptoms
Managing paresthesia often requires flexibility in treatment approaches. As symptoms evolve, it’s crucial to revisit and adjust your management plan accordingly. Regular consultations with healthcare providers can help identify the most effective strategies tailored to current experiences.
Medications may need modification as symptoms change. For instance, dosages might require adjustment, or alternative medications may be introduced based on effectiveness or side effects. Staying informed about new treatments is essential for making educated choices.
Physical therapy can also play a significant role in symptom management. As your condition progresses, specific exercises or techniques may become more beneficial than others. Working closely with a physical therapist ensures you target the right areas and promote healing effectively.
Lifestyle changes should not be overlooked either. Incorporating stress-reduction techniques like mindfulness or yoga can alleviate discomfort associated with paresthesia. Tracking triggers helps individuals understand what exacerbates their symptoms and allows for better control over their daily lives.
Quality of Life Impact: Managing Progressive Paresthesia
Living with progressive paresthesia can significantly affect daily life. Many individuals experience disruptions in their routines due to numbness, tingling, or other sensory changes. This discomfort may lead to challenges in performing simple tasks like typing, walking, or even holding objects.
Mental health is also impacted by these symptoms. Anxiety and frustration often arise when sensations worsen or become unpredictable. Feeling out of control over one’s body can create additional stress that compounds the already challenging physical aspects of the condition.
Finding effective coping strategies becomes essential for maintaining quality of life. Engaging in mindfulness practices such as yoga and meditation can release tension and enhance emotional well-being. Support groups provide a space for sharing experiences and receiving encouragement from others who understand similar struggles.
Open communication with healthcare providers helps tailor management plans according to individual needs. Regular check-ins ensure adjustments are made promptly, promoting better symptom control and enhancing overall life satisfaction despite the ongoing challenges posed by paresthesia.
Research Insights: Future Perspectives on Slowing Progression
As research continues to evolve, there are exciting developments on the horizon for understanding and managing paresthesia. Advances in neuroscience have led to a deeper comprehension of nerve function and regeneration. This knowledge can aid in identifying potential treatments that target the underlying causes of paresthesia symptoms.
Emerging therapies, including neuroprotective agents and regenerative medicine techniques, show promise in slowing symptom progression. Researchers are also exploring genetic factors that contribute to individual experiences with paresthesia. Tailoring treatment options based on genetic profiles could lead to more effective management strategies.
Furthermore, studies focusing on lifestyle modifications highlight the importance of diet, exercise, and stress management as integral components of care plans. These findings suggest that proactive measures may not only alleviate current symptoms but also help prevent future complications.
Staying informed about ongoing research is crucial for those affected by paresthesia. Engaging with healthcare professionals who specialize in this area will ensure access to the latest treatment options and support networks dedicated to improving quality of life for patients experiencing progressive symptoms.


