Introduction to Skin Biopsy in Paresthesia Diagnosis
Paresthesia, the tingling or numbness that can disrupt daily life, often leaves patients and doctors searching for answers. While many may turn to traditional diagnostic methods like MRI or nerve conduction studies, there’s a lesser-known tool gaining traction in this field: the skin biopsy. This seemingly simple procedure offers valuable insights into nerve health and function.
When conventional tests fall short, a skin biopsy can shine a light on underlying causes of paresthesia. By examining small samples of skin tissue, healthcare professionals can identify abnormalities that point toward specific neurological disorders. Understanding how this innovative approach works could pave the way for better diagnosis and treatment options for those grappling with unexplained sensations.
Join us as we dive deeper into the world of skin biopsies—an underappreciated yet powerful ally in diagnosing paresthesia—and learn when it might be recommended, what to expect during the procedure, and how results are interpreted to help guide your care journey.
When is a Skin Biopsy Recommended for Paresthesia?
A skin biopsy is often recommended when a patient experiences unexplained paresthesia, which includes sensations like tingling or numbness. If neurological tests do not yield clear results, this procedure can provide valuable insights into nerve function.
When symptoms suggest possible small fiber neuropathy or other peripheral nerve disorders, a skin biopsy becomes an essential tool. It allows doctors to assess the density of nerve fibers in the skin, helping pinpoint underlying issues that standard tests might miss.
Patients with chronic conditions such as diabetes or autoimmune diseases may also benefit from a skin biopsy. In these cases, it helps determine if nerve damage has occurred due to their illness.
If you have persistent symptoms and your healthcare provider cannot find answers through conventional methods, discussing a skin biopsy could be worthwhile. This diagnostic approach can uncover critical information about your nerve health.
Types of Skin Biopsies Used in Neurological Diagnosis
Skin biopsies are essential in diagnosing various neurological conditions, especially when evaluating paresthesia. There are several types of skin biopsy techniques used to obtain tissue samples.
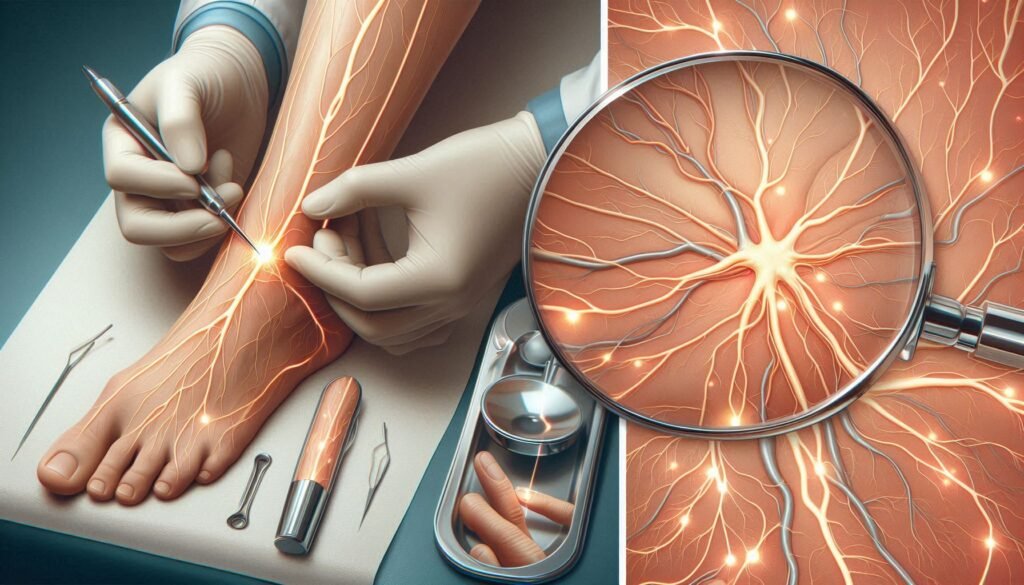
The most common type is the punch biopsy. This method utilizes a circular blade to remove a small cylindrical section of skin. It’s minimally invasive and often performed under local anesthesia, allowing for quick recovery.
A shave biopsy is another technique employed in certain cases. Here, the dermatologist removes only the superficial layers of skin using a scalpel or razor-like instrument. While less invasive than other methods, it may not capture deeper nerve fibers crucial for diagnosing neuropathies.
Incisional biopsies involve removing a larger portion of tissue from an area experiencing symptoms. This approach can provide more comprehensive information about underlying conditions but may require stitches and longer healing times. Each method has its specific applications based on individual patient needs and suspected diagnoses.
The Skin Biopsy Procedure: What to Expect
When you arrive for a skin biopsy, the process begins with an assessment by your healthcare provider. They will explain the procedure in detail and address any concerns you may have. It’s important to feel comfortable before proceeding.
Next, your doctor will clean the area where the biopsy will occur. A local anesthetic is then administered to numb the site. You might feel a slight pinch or sting as it’s injected, but this sensation should dissipate quickly.
Once the area is numbed, your doctor will use specialized tools to remove a small sample of skin tissue. The type of tool used depends on the specific biopsy technique selected—punch, shave, or excisional methods are common options.
After obtaining the sample, pressure may be applied to stop any bleeding. Sterile dressing will cover the site to protect it during healing. This entire process usually takes less than 30 minutes and allows patients to return home shortly afterward.
Analyzing Skin Biopsy Samples: Epidermal Nerve Fiber Density
Analyzing skin biopsy samples focuses significantly on epidermal nerve fiber density (ENFD). This measurement assesses the number of small nerve fibers present in the skin’s outer layer, providing insight into peripheral nerve health.
A reduced ENFD can indicate neuropathies, which are often associated with conditions like diabetes or autoimmune diseases. An accurate assessment is crucial for diagnosing underlying issues that could be causing paresthesia symptoms.
Lab technicians typically use specialized staining techniques to visualize these nerve fibers under a microscope. The process allows them to count and evaluate the density of nerves accurately, revealing critical information about possible damage or degeneration.
Understanding ENFD results is essential for healthcare providers as it guides further diagnostic processes and treatment decisions. A high level of awareness about this analysis contributes to better patient care in managing neurological disorders tied to paresthesia.
Interpreting Skin Biopsy Results: What They Reveal About Nerve Health
Interpreting skin biopsy results can provide valuable insights into nerve health, particularly for those experiencing paresthesia. A key metric analyzed is the epidermal nerve fiber density (ENFD). This measures the number of small nerve fibers present in a specific area of skin.
Low ENFD levels often indicate peripheral neuropathy, which can manifest as tingling, numbness, or pain. Conditions like diabetes or autoimmune disorders may be identified through these findings. By assessing changes in ENFD over time, healthcare providers can track disease progression and treatment effectiveness.
Conversely, normal ENFD results suggest that other factors might be contributing to paresthesia symptoms. It may lead clinicians to explore different diagnostic avenues or consider non-neurological causes.
The interpretation process requires expertise since variations can occur due to various reasons such as age or localized conditions. Collaboration between dermatologists and neurologists enhances accuracy in determining diagnosis based on biopsy outcomes.
Benefits and Limitations of Skin Biopsy in Paresthesia Diagnosis
Skin biopsy serves as a valuable tool in diagnosing paresthesia. It allows for the direct examination of nerve fibers in the skin, providing insights into conditions that may not be evident through other methods. This technique can reveal abnormalities like reduced epidermal nerve fiber density, helping pinpoint underlying neuropathies.
One significant benefit is its minimally invasive nature. Compared to more complex procedures such as electromyography or imaging studies, skin biopsies require only local anesthesia and typically have shorter recovery times. Patients often experience less discomfort and can return to their normal activities quickly.
However, limitations exist with this diagnostic approach. The sample size is relatively small, which might miss diffuse or widespread nerve damage. Additionally, interpretation of results relies heavily on experienced pathologists who must differentiate between various forms of neuropathy effectively.
Moreover, while skin biopsy provides essential information about peripheral nerves, it does not address central nervous system issues directly related to paresthesia symptoms. Thus, it’s one piece of a larger diagnostic puzzle.
Comparing Skin Biopsy to Other Diagnostic Methods
Skin biopsy stands out among diagnostic methods for paresthesia due to its ability to directly assess nerve health. Unlike traditional imaging techniques, such as MRI or CT scans, which visualize structural abnormalities, a skin biopsy provides cellular-level insights. This is particularly useful in diagnosing small fiber neuropathy, often responsible for tingling and numbness.
Electromyography (EMG) and nerve conduction studies are other common tests used in evaluating nerve function. While these methods measure electrical activity and signal transmission, they may not detect early or subtle changes that a skin biopsy can reveal. The latter focuses on the density of epidermal nerve fibers, offering crucial information about peripheral nerves.
Furthermore, skin biopsies are minimally invasive and typically performed under local anesthesia. This contrasts with more complex procedures like lumbar punctures that carry greater risk and discomfort.
Each diagnostic method has its strengths; however, the unique capabilities of a skin biopsy make it an important tool when investigating unexplained sensations in patients with paresthesia.
Potential Risks and Side Effects of Skin Biopsy
While a skin biopsy is generally safe, it does come with potential risks and side effects. One of the most common concerns is bleeding at the biopsy site. Although this usually resolves quickly, some individuals may experience prolonged bleeding that requires medical attention.
Infection is another possible complication. The procedure involves breaking the skin barrier, which increases vulnerability to bacteria. Proper aftercare can mitigate this risk, but it’s essential to monitor for signs of infection such as increased redness or pus.
Scarring can also occur following a skin biopsy. The extent varies depending on individual healing processes and the size of the incision made during the procedure. Some people may develop hypertrophic scars or keloids if they are prone to abnormal scarring.
Patients might experience temporary discomfort or pain in the area where biopsies were taken. This sensation typically subsides within days but can be managed with over-the-counter pain relief if needed.
Follow-Up Care and Treatment Planning After Skin Biopsy Results
After receiving skin biopsy results, the next steps involve careful consideration and planning for treatment. Your healthcare provider will discuss the findings with you and what they mean for your specific condition. If nerve damage or abnormalities are detected, a personalized treatment plan can be developed.
Follow-up care may include physical therapy to improve mobility and function, medications to manage pain or discomfort, and lifestyle changes that promote nerve health. In some cases, further testing might be necessary to rule out other underlying conditions contributing to paresthesia.
Regular follow-up appointments will ensure that your progress is monitored closely. Communication with your healthcare team is crucial during this time; don’t hesitate to ask questions about the implications of your biopsy results or any concerns you may have regarding the recommended treatments.
Understanding how skin biopsies fit into the broader framework of diagnosing paresthesia allows patients to take active roles in their health decisions. With proper support and tailored interventions based on biopsy outcomes, many individuals can find relief from symptoms while improving their quality of life.


