Paresthesia in Multiple Sclerosis: A Distinct Subtype is a complex and often misunderstood aspect of living with this chronic condition. For many individuals, the sensation of tingling, numbness, or crawling sensations can be alarming and disruptive to daily life. As part of the broader neurological landscape that defines multiple sclerosis (MS), paresthesia serves as both a symptom and an indicator of how deeply MS affects the nervous system.
Understanding how these sensations manifest helps patients navigate their experiences better. Commonly described as “pins and needles,” paresthetic symptoms can vary widely from person to person. They may even change over time or fluctuate in intensity based on various triggers.
In this blog post, we will delve deeper into what causes these unusual sensations within the context of MS, explore common experiences reported by patients, assess diagnostic methods used in identifying these symptoms, and discuss treatment options available for management. Join us as we uncover the intricate relationship between paresthesia and multiple sclerosis while providing insights that empower those affected by this distinct subtype.
Understanding Paresthesia as a Symptom of Multiple Sclerosis
Paresthesia is a common symptom experienced by individuals with multiple sclerosis (MS). It refers to abnormal sensations such as tingling, prickling, or numbness that can occur anywhere in the body. Many describe these feelings as “pins and needles,” often impacting their quality of life.
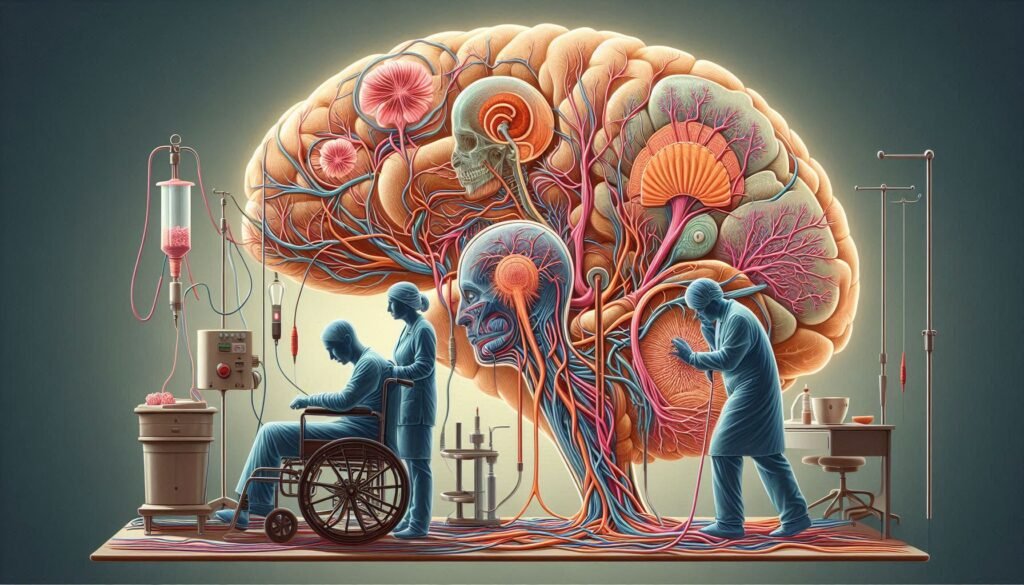
In MS, paresthesia arises due to damage to the myelin sheath—the protective covering around nerve fibers. This demyelination disrupts normal electrical signals within the nervous system. As a result, sensory messages become distorted or miscommunicated.
The onset of paresthetic symptoms can be sudden and may fluctuate in intensity. Some patients experience them consistently, while others face intermittent episodes triggered by factors like stress or temperature changes.
Understanding this symptom is crucial for both patients and healthcare professionals alike. Recognizing how it affects daily activities allows for better coping strategies and tailored treatment options moving forward.
How MS Affects the Nervous System to Cause Paresthesia
Multiple sclerosis (MS) is an autoimmune disorder that disrupts the central nervous system. It occurs when the immune system mistakenly attacks myelin, the protective sheath covering nerve fibers. This damage results in communication breakdown between the brain and various body parts.
When myelin is damaged, it can lead to a range of sensory disturbances, including paresthesia. As electrical signals struggle to travel along affected nerves, sensations such as tingling or numbness may arise. The severity and location of these symptoms depend on which nerves are impacted.
In MS patients, lesions form in different areas of the brain and spinal cord. These lesions interfere with normal signaling pathways, resulting in altered sensory experiences. For many individuals living with MS, paresthesia serves as one of their first signs.
The unpredictable nature of these symptoms adds complexity to daily life for those diagnosed with MS. Understanding how this condition affects nerve function is crucial for managing and mitigating its impact on overall well-being.
Common Paresthesia Sensations Experienced by MS Patients
Paresthesia in multiple sclerosis can manifest in various sensations that significantly impact daily life. Patients often report feelings of tingling or “pins and needles” that may occur in different parts of the body, particularly in the limbs. This sensation can be fleeting or persistent, making it difficult to predict when it will strike.
Another common experience is numbness, which might affect one side of the body more than the other. This loss of feeling can lead to challenges with coordination and balance, increasing the risk of falls. Many individuals note that these episodes sometimes worsen during physical activity or stress.
Some MS patients describe a burning sensation along their skin, adding an additional layer of discomfort. This peculiar warmth can feel localized or widespread, complicating their ability to engage comfortably in everyday activities.
Additionally, there are instances where patients experience electric shock-like sensations when moving their heads. Known as Lhermitte’s sign, this symptom highlights how diverse paresthesia manifestations can be within the context of multiple sclerosis.
Triggers and Exacerbating Factors for MS-Related Paresthesia
Multiple sclerosis-related paresthesia can be influenced by various triggers and exacerbating factors. Stress is a significant contributor, as it can amplify symptoms. Patients often report heightened sensations during stressful situations or emotional upheaval.
Temperature changes play a crucial role in the experience of paresthesia. Many individuals with MS are sensitive to heat, which can worsen their symptoms. Even warm weather or hot baths may lead to an increase in tingling sensations.
Fatigue also significantly affects how patients perceive paresthesia. As energy levels drop, nerve function may decline, leading to more pronounced sensory disturbances. Ensuring adequate rest becomes vital for managing these symptoms effectively.
Certain medications and lifestyle choices can exacerbate paresthesia too. Caffeine intake, alcohol consumption, and some prescription drugs might heighten discomfort for some people with MS. Understanding personal triggers allows patients to better manage their experiences with this complex symptom.
Diagnostic Approaches: Identifying MS-Induced Paresthesia
Diagnosing paresthesia in multiple sclerosis (MS) involves a thorough assessment of symptoms and medical history. Neurologists typically start with a detailed discussion, focusing on the nature of the sensations experienced by the patient. Common descriptions include tingling, numbness, or a prickly feeling.
Next, neurological examinations are crucial to evaluate reflexes, muscle strength, and coordination. These assessments help identify any physical abnormalities that may indicate nerve damage associated with MS. Advanced imaging techniques like magnetic resonance imaging (MRI) are often employed as well to visualize lesions in the brain or spinal cord.
Electromyography (EMG) and nerve conduction studies can further assist in understanding how signals travel through nerves affected by MS. These tests measure electrical activity in muscles and assess the speed at which impulses move through nerves.
A diagnosis is usually made based on clinical findings combined with test results. This comprehensive approach ensures that other potential causes for paresthesia are ruled out before attributing symptoms specifically to multiple sclerosis.
Treatment Options for Managing Paresthesia in MS Patients
Managing paresthesia in multiple sclerosis patients often requires a multifaceted approach. Healthcare providers typically begin with assessing the severity and frequency of symptoms, tailoring treatment strategies accordingly. Medications such as anticonvulsants or antidepressants can help alleviate nerve pain and discomfort associated with these sensations.
Physical therapy plays a crucial role in enhancing mobility and reducing muscle tension. Targeted exercises can improve overall function while minimizing the impact of paresthesia on daily activities. Occupational therapy may also provide adaptive techniques to cope with everyday tasks more easily.
Lifestyle modifications can significantly influence symptom management as well. Stress reduction through mindfulness practices or yoga has shown promise for many patients seeking relief from overwhelming sensations. Additionally, maintaining proper hydration and nutrition is vital for overall neurological health.
Alternative therapies like acupuncture or biofeedback have garnered interest among those looking for supplemental options beyond conventional treatments. Always consult healthcare professionals before making any changes to your treatment plan to ensure safety and effectiveness.
The Role of Disease-Modifying Therapies in Reducing Paresthesia
Disease-modifying therapies (DMTs) play a crucial role in managing multiple sclerosis and its associated symptoms, including paresthesia. By targeting the underlying disease process, DMTs can help reduce the frequency and severity of relapses. This reduction is significant because it may directly impact the occurrence of paresthetic sensations.
These treatments work by modulating the immune system to prevent it from attacking myelin—the protective sheath around nerve fibers. With less damage to nerves, many patients report a decrease in abnormal sensations like tingling or numbness. The effectiveness of DMTs varies among individuals, but many find relief from their symptoms over time.
Some commonly used DMTs include interferons and monoclonal antibodies. Each has distinct mechanisms that contribute to overall symptom management. It’s essential for patients to discuss with their healthcare providers which option might be most beneficial based on their specific situation.
Additionally, ongoing research continues to unveil new therapies aimed at not only slowing down disease progression but also alleviating discomfort caused by paresthesia. This evolving landscape offers hope for better quality of life for those living with MS.
Coping Strategies for Daily Life with MS-Related Paresthesia
Living with paresthesia as a symptom of multiple sclerosis can be challenging, but there are effective coping strategies that can help improve daily life. First, maintaining a structured routine can provide stability. Regular schedules for meals, sleep, and activities enhance predictability and reduce anxiety associated with sudden symptoms.
Second, practicing mindfulness techniques such as meditation or deep breathing exercises may alleviate stress. These practices promote relaxation and allow individuals to focus on the present moment rather than dwelling on discomfort.
Incorporating gentle physical activity into your day is essential too. Activities like yoga or swimming not only boost mood but also enhance circulation, which could ease sensations of tingling or numbness.
Consider joining support groups where you can connect with others facing similar challenges. Sharing experiences fosters understanding and provides emotional relief while equipping you with practical tips from fellow MS patients who understand what you’re going through.
Distinguishing MS Paresthesia from Other Neurological Causes
Paresthesia in Multiple Sclerosis can often be mistaken for other neurological conditions. Conditions such as neuropathy, stroke, or even anxiety disorders may present similar symptoms like tingling or numbness. It’s crucial to recognize the unique characteristics of MS-related paresthesia.
One distinguishing feature is its episodic nature. MS patients frequently report sensations that appear and disappear unexpectedly. This contrasts with more persistent symptoms seen in conditions like diabetic neuropathy, where sensations tend to remain constant over time.
Moreover, the location of paresthesia can also provide clues. In MS, it commonly affects specific areas related to demyelinated lesions in the central nervous system. Identifying these patterns is essential for accurate diagnosis.
A detailed medical history and neurological examination play vital roles in differentiation. Healthcare providers look at symptom duration and triggers while considering patient history to rule out alternative causes effectively.
Latest Research on Paresthesia Management in Multiple Sclerosis
Recent research has shed light on the complexities of paresthesia in multiple sclerosis and how to manage it effectively. Studies have focused on understanding the underlying mechanisms that lead to these sensations, which can greatly enhance treatment approaches.
Emerging therapies aim to target nerve pathways more precisely, offering new hope for patients experiencing debilitating symptoms. Clinical trials are exploring novel medications and interventions that may reduce the frequency or intensity of paresthesia episodes.
Additionally, researchers are investigating non-pharmacological options such as physical therapy and cognitive behavioral strategies. These methods help empower patients by providing tools to cope with their symptoms better.
As science continues to advance, so does our knowledge of MS-related paresthesia. With ongoing studies analyzing patient-reported outcomes, there is optimism for developing comprehensive care plans tailored specifically for those affected by this unique aspect of multiple sclerosis. Staying informed about these developments can be crucial for both patients and healthcare providers alike.


