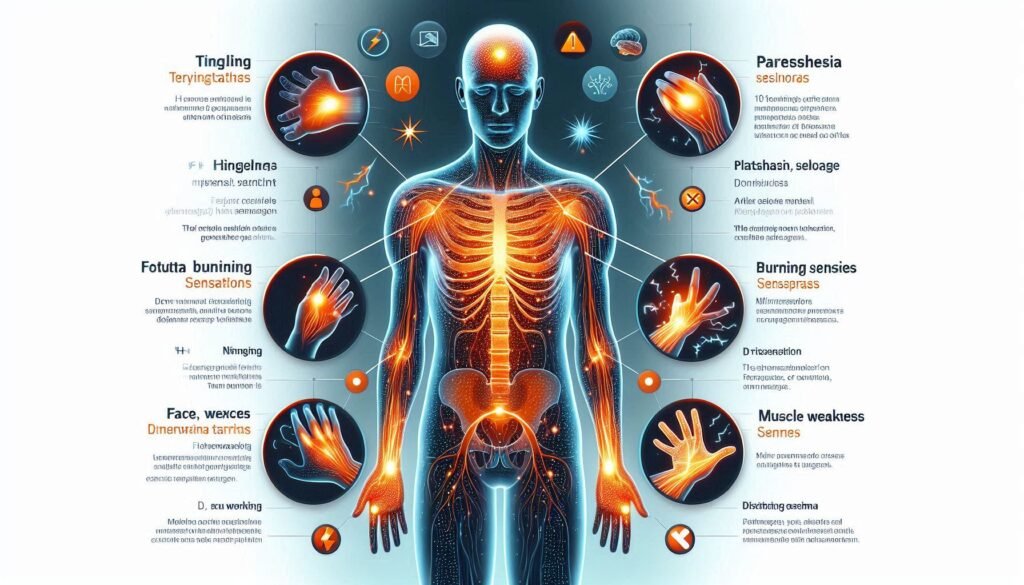
Paresthesia is a term that may sound unfamiliar, but it describes sensations many of us have experienced at some point in our lives. From the tingling feeling when your foot “falls asleep” to unexplained numbness in your fingers, paresthesia can be both puzzling and concerning. While occasional episodes are usually harmless, certain symptoms should never be ignored.
Understanding common paresthesia symptoms can empower you to take proactive steps toward your health. So, what exactly should you look out for? In this essential guide, we’ll explore ten critical symptoms of paresthesia that warrant attention. Equip yourself with knowledge and learn how to recognize signs that could indicate an underlying issue requiring medical intervention. Your body communicates with you—let’s make sure you’re listening!
Understanding Paresthesia: A Brief Overview
Paresthesia refers to abnormal sensations in the skin, often described as tingling, prickling, or numbness. These sensations can occur anywhere on the body but are most commonly felt in the hands and feet. While paresthesia itself isn’t a condition, it is often a symptom of other underlying issues.
The causes of paresthesia vary widely. They may include nerve compression from prolonged pressure on nerves, peripheral neuropathy due to diabetes, vitamin deficiencies, or even anxiety. Certain medical conditions like multiple sclerosis and stroke can also trigger these sensations.
Duration plays an important role in understanding paresthesia’s significance. Temporary episodes usually resolve quickly without treatment; however, persistent symptoms merit further investigation by healthcare professionals.
Recognizing when paresthesia occurs alongside other concerning signs is crucial for timely intervention. Understanding this phenomenon helps individuals better communicate their experiences with doctors and seek appropriate care when necessary.
Tingling Sensations: The Hallmark of Paresthesia
Tingling sensations, often described as a prickling or “pins and needles” feeling, are among the most recognizable symptoms of paresthesia. These sensations can occur in various parts of the body but are commonly felt in the hands, feet, arms, and legs. They may arise suddenly or develop gradually over time.
This hallmark symptom is typically caused by nerve compression or irritation. For instance, sitting cross-legged for extended periods can compress nerves in your legs, leading to that familiar tingling sensation when you stand up. However, persistent tingling without a clear cause could signal an underlying issue.
In some cases, tingling might accompany other symptoms like numbness or weakness. It’s crucial to pay attention to how long these sensations last and whether they recur frequently. If tingling continues without improvement or worsens over time, seeking medical advice is essential.
Understanding this symptom better allows patients to distinguish between normal occurrences and those needing further investigation by a healthcare professional.
Numbness in Extremities: When to Seek Medical Attention
Numbness in the extremities can be more than just an uncomfortable sensation. It often signals a disruption in nerve function, which can stem from various underlying health issues. If you experience numbness that persists for more than a few minutes or occurs frequently, it’s essential to take notice.
Accompanying symptoms are equally important indicators. Look out for sudden onset numbness alongside weakness, confusion, or difficulty speaking. These could suggest serious conditions like stroke and warrant immediate medical attention.
Additionally, if numbness follows an injury—especially to the spine or neck—it’s crucial to seek help promptly. Damage during such incidents may lead to long-term complications if not addressed quickly.
Chronic conditions such as diabetes or multiple sclerosis can also manifest through numbness. Regular check-ups with your healthcare provider will help monitor these symptoms effectively and ensure appropriate management of any underlying issues.
Burning Sensations: A Critical Symptom to Monitor
Burning sensations can be alarming and often indicate underlying issues in the nervous system. These feelings might arise spontaneously or after specific activities, such as prolonged sitting or repetitive motions. If you experience this symptom frequently, it’s essential to pay attention.
The burning sensation may occur in various parts of the body, primarily affecting hands, feet, and legs. This discomfort can stem from nerve damage due to conditions like diabetes or multiple sclerosis. Identifying patterns related to your symptoms is crucial for accurate diagnosis.
Many patients describe these sensations as if their skin is on fire or experiencing a hot flash. It could also feel like an intense itch that doesn’t subside with scratching. Keeping track of when these episodes happen will provide valuable information for healthcare providers.
If the burning persists or worsens over time, seeking medical advice becomes imperative. Early intervention can lead to better outcomes and prevent further complications.
Pins and Needles Feeling: Differentiating Normal from Abnormal
The pins and needles feeling, often described as tingling or prickling sensations, is a common experience for many. This sensation usually occurs when pressure is applied to nerves, such as sitting in one position for an extended time. Once the pressure is relieved, normal sensation typically returns.
However, not all instances of this feeling are benign. If you frequently experience pins and needles without any obvious cause or after minor activities, it could signal an underlying issue. Conditions like diabetes or nerve damage may lead to persistent symptoms that warrant further evaluation.
Pay attention to the duration and frequency of these sensations. Occasional episodes can be harmless; however, if they become chronic or are accompanied by other alarming symptoms—such as weakness or loss of coordination—it’s essential to seek medical advice promptly.
Differentiating between normal and abnormal sensations can help you take control of your health. Awareness plays a crucial role in preventing potential complications down the line.
Muscle Weakness Associated with Paresthesia
Muscle weakness can be a concerning symptom associated with paresthesia. It often manifests alongside tingling or numbness, signaling potential underlying issues. When you experience muscle weakness in conjunction with these sensations, it may indicate nerve compression or damage.
This symptom can affect your ability to perform daily tasks. Simple actions like picking up objects or even walking might feel more challenging than usual. The combination of weakness and paresthesia can lead to frustration and diminished quality of life.
It’s crucial to monitor how long the muscle weakness persists. If it lasts for an extended period or worsens over time, seeking medical attention is essential. A healthcare professional can conduct tests to determine the root cause and recommend appropriate treatment options.
Understanding this association between muscle weakness and paresthesia empowers patients to take proactive steps toward their health. Early intervention could mitigate further complications, making awareness vital for anyone experiencing these symptoms.
Increased Sensitivity to Touch: Hyperesthesia in Paresthesia
Increased sensitivity to touch, known as hyperesthesia, is a critical symptom associated with paresthesia. Individuals experiencing this condition may find that even light touches feel intense or uncomfortable. This heightened sensitivity can significantly impact daily activities and overall quality of life.
Hyperesthesia often occurs alongside other paresthesia symptoms, such as tingling or numbness. The combination can create an overwhelming sensation that disrupts normal function. Simple tasks like wearing clothes or shaking hands may become challenging due to the discomfort involved.
The underlying causes of hyperesthesia vary widely, ranging from nerve damage to systemic conditions such as diabetes or multiple sclerosis. Identifying the root cause is vital for effective management and treatment options tailored to individual needs.
If you notice an increase in sensitivity to touch along with other abnormal sensations, it’s essential not to ignore these signs. Consulting a healthcare professional will provide clarity on your symptoms and appropriate interventions for relief.
Temperature Perception Changes: Hot and Cold Sensitivities
Temperature perception changes can be a subtle yet alarming symptom of paresthesia. Many patients report feeling unusual sensitivity to hot and cold temperatures. This heightened awareness can lead to discomfort or confusion when exposed to different environmental conditions.
For some, a mild temperature may feel unbearably hot, while others might struggle to detect warmth at all. These variations are not just annoying; they can affect daily life significantly. Activities such as showering or spending time outdoors become challenging when you can’t trust your body’s signals.
In some cases, these sensitivities stem from nerve damage or issues with the central nervous system. Conditions like multiple sclerosis or diabetes often present with altered temperature perception as a prominent symptom.
Recognizing these changes is essential for effective management and treatment options. If you notice significant differences in how your body responds to heat and cold, it’s crucial to consult a healthcare provider for further evaluation and support.
Coordination Issues: Balance and Fine Motor Skill Challenges
Coordination issues can significantly impact daily life, especially when linked to paresthesia. Individuals may experience difficulty with balance and fine motor skills. Simple tasks like buttoning a shirt or writing can become frustrating challenges.
These symptoms often arise because the nerves that control movement are affected. When these signals are disrupted, it leads to clumsiness or unsteady movements. You might notice yourself stumbling more frequently or having trouble holding objects firmly.
Balance problems can also pose risks, increasing the likelihood of falls and injuries. This is particularly concerning for older adults who may already have mobility issues. Maintaining stability becomes crucial in preventing accidents.
If you find yourself struggling with coordination alongside other paresthesia symptoms, it’s essential to consult a healthcare professional. They can help identify the underlying cause and recommend appropriate treatments or therapies tailored to your needs.
Pain and Discomfort: When Paresthesia Becomes Painful
Paresthesia can often present as a benign sensation. However, when it escalates to pain and discomfort, it’s time to take notice. Pain associated with paresthesia may manifest in various forms—sharp, throbbing, or even aching sensations that disrupt daily life.
If you experience persistent pain alongside tingling or numbness, this could indicate an underlying condition requiring prompt medical intervention. Conditions such as neuropathy or herniated discs can produce these uncomfortable symptoms. Ignoring these signals might lead to further complications down the line.
Pay attention if your pain intensifies over time or affects your ability to perform everyday tasks. Seeking professional advice is critical for proper diagnosis and treatment options tailored to your needs. Remember, understanding and addressing common paresthesia symptoms you shouldn’t ignore can pave the way for effective management of your health concerns. Taking action sooner rather than later ensures a better quality of life moving forward.


